The Changing Response to AIDS
A neglected global health crisis ultimately became a top priority for policymakers, donors, and doctors.

A giant red ribbon hangs from the North Portico of the White House to mark World AIDS Day on December 1, 2013, in Washington.
Source: Mike Theiler/Reuters
Teaching Resources—Global Health: Policy (including lesson plan with slides)
Higher Education Discussion Guide
HIV/AIDS is one of the deadliest communicable diseases of the modern era: approximately thirty-three million people have perished from AIDS-related illnesses. The U.S. government and international organizations now commit significant resources to preventing and treating HIV/AIDS. However, this was not always the case. This timeline traces the evolution of patient activism, scientific research, international attitudes, and public policy that eventually converged to create the coordinated international HIV/AIDS effort that exists today.
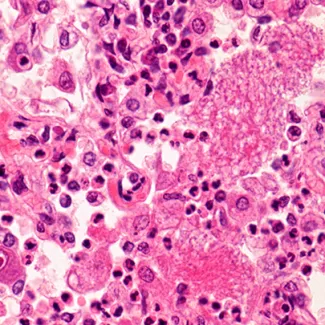
In the early 1900s, a version of the virus that would become known as the human immunodeficiency virus (HIV) was transferred from chimpanzees. This transfer to humans occurred through the food supply somewhere near the Congo River. It traveled across the then Belgian Congo to Europe and eventually found its way to the United States around 1969. Exactly how many people were infected with or died because of HIV before then is unknown. No definitive health record–keeping infrastructure existed in many African countries. Moreover, other health issues masked its spread. HIV’s long incubation period means the virus can spend more than fifteen years attacking a person’s immune system before progressing into its final and most severe stage: AIDS. Even in the United States, AIDS only surfaced more than a decade after its arrival. The virus was first detected among the gay populations in California and New York in 1981.

American Museum of Natural History via Flickr
American Museum of Natural History via Flickr
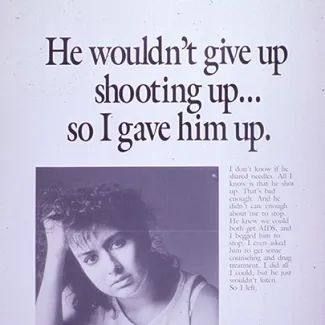
Wellcome Collection under CC0
The Centers for Disease Control (CDC) received a report that five otherwise healthy gay men in Los Angeles had suddenly come down with pneumocystis pneumonia. This infection is one that any healthy person’s immune system should be able to easily fight off. Within days, the CDC was flooded with similar cases from all over the country. Because the first cases of the illness were documented in gay men in the United States, people called it GRID (gay-related immune deficiency), gay cancer, or the gay plague. This stigma assigned to AIDS and the gay community would make the spread of the illness even harder to stop for decades to come.
CDC via U.S. National Library of Medicine
The CDC used the name AIDS (acquired immune deficiency syndrome) for the first time to describe the mysterious illness in 1982. Cases had been detected in homosexual people, people with hemophilia (a bleeding disorder), Haitians, and heroin users. Infections across these demographics led the public to ridicule these communities as the 4-H Club. Health officials also recorded symptoms now believed to be associated with AIDS in patients in Uganda; at the time, no one on either side of the ocean made the connection. It would take until 1986 for even the cause of AIDS, the retrovirus HIV, to be confirmed and named.

Antonin Cermak/Fairfax Media via Getty Images
Scientists were still unsure of exactly how easily HIV was transmitted, but the CDC was fairly certain that it traveled by blood. (Today, we know that certain activities where bodily fluids are exchanged raise a person’s risk of contracting HIV.) As recipients of blood transfusions, such as people with hemophilia, started to rapidly fall ill, the CDC workers met their counterparts at blood banks to urge them to screen the entire blood supply. No test was available for AIDS specifically, but an existing test for Hepatitis B proved to be a good substitute. If the blood tested positive for Hepatitis B, 88 percent of the time its donor also had AIDS. Wary of the cost of administering so many tests and demanding more evidence of contamination, the blood banks refused. As a result, almost half of the ten thousand people with hemophilia living in the United States contracted AIDS. Four thousand would later die.
Rick Maiman/AP
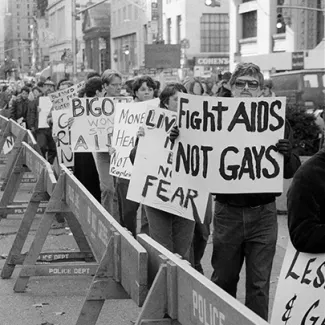
At the National Lesbian and Gay Health Conference in Denver, Colorado, the National Association of People with AIDS (NAPWA) was founded. In an unprecedented move for patient rights, the association adopted the Denver Principles articulating the rights of people with AIDS. These principles included the rights “to privacy, to confidentiality of medical records, to human respect”—language that paved the way for many of the legal rights all patients have today. These weren’t just medical rights. At a time when people with AIDS were stigmatized and marginalized, the Denver Principles affirmed their humanity. Years later, the Denver Principles would inspire South African activists to form their own NAPWA. This organization would become instrumental in the fight against AIDS in their own country.

Reuters
Dr. Robert Gallo and his team of researchers from the National Institutes of Health published a report claiming that they had isolated the retrovirus that causes AIDS. This report followed a similar finding from the Institut Pasteur of France a year earlier. Both teams believed their virus was the cause of AIDS. Only in 1986 would scientists discover that both viruses were, in fact, the same entity and name it the human immunodeficiency virus (HIV). A public (and at times, vitriolic) patent fight over who discovered the retrovirus first quickly ensued between U.S. and French labs. This patent battle gave many people with AIDS the impression that the scientific community was more interested in claiming credit than finding effective treatment.
U.S. National Library of Medicine
A 12-year-old boy named Ryan White was diagnosed with AIDS, transmitted via contaminated blood products. A year later, White was denied entry to his school by the superintendent because parents complained he might infect their children. Many of these same parents pulled their children out of school when a court finally ordered that White be allowed back. Ryan and his mother would go on to become national advocates for people with AIDS. Although the media called him an innocent victim, he forcefully rejected that language. White was determined to dispel the implication that other people with AIDS were somehow guilty.

Courtesy of Lambda Archives of San Diego
By the end of 1984, 11,152 AIDS cases had been reported in the United States.762 cases had been reported in Europe. However, the disease was not limited to these areas. AIDS was also traveling across Africa. Later research revealed that in 1984 nearly two million people in Africa were living with HIV. By 1990, over one million people there had succumbed to AIDS.
The American actor Rock Hudson died from AIDS in 1985. Until then, President Ronald Reagan had never uttered the word AIDS in public. Rather, his press secretary had responded to questions about AIDS with jokes about homosexuality. But Hudson’s death gave AIDS a familiar face. His popularity, coupled with the prolonged efforts of activists, spurred the United States to start taking steps to address the issue domestically. In 1985, the U.S. Congress allocated $70 million to AIDS research. This move came four years after researchers at the Centers for Disease Control (CDC) had proposed allocating $40 million to head off the virus early on. However, the CDC was given less than $1 million.

Office of Speaker of the House Nancy Pelosi via Flickr under CC BY 2.0
Office of Speaker of the House Nancy Pelosi via Flickr under CC BY 2.0
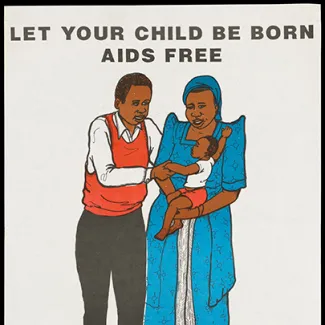
STD/AIDS Control Programme of the Ministry of Health of Uganda via Wellcome Collection under CC BY-NC 4.0
With the help of the World Health Organization, Uganda became the first African country to start an AIDS control program. However, Uganda was the exception on the continent. Studies found alarming rates of infection in the Democratic Republic of Congo, but European researchers were focused primarily on showing that AIDS came from Africa instead of offering solutions to the crisis. The stigma around AIDS and homosexuality made African governments and even scientists resistant to counting the number of people affected. These African nations feared that the association with homosexuality would make tourism decline. Uganda’s destigmatizing and educational approach made it one of the first countries to be successful at turning back the epidemic. While rates of HIV prevalence were rising across the continent, the rate in Uganda began declining in 1992.

Bettmann Archive via Getty Images
After the virus that caused AIDS was named, a test for HIV was approved by the U.S. Food and Drug Administration. Three years after their initial refusal, the American Association of Blood Banks and the Red Cross finally began screening the country’s blood supply for HIV. Blood banks rejected gay donors, a policy that still informs who is eligible to give blood today.
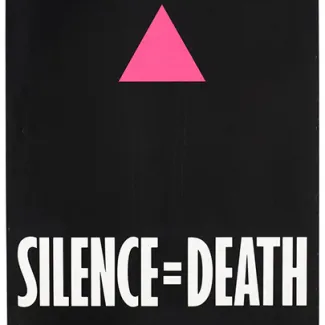
ACT-UP, The AIDS Coalition To Unleash Power via Wellcome Collection under CC BY-NC 4.0
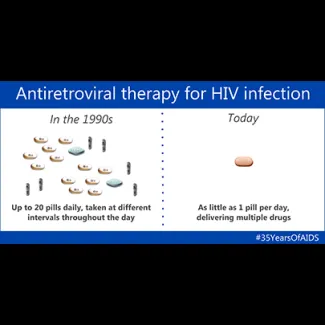
Azidothymidine (AZT) became the first anti-HIV drug approved by the U.S. Food and Drug Administration (FDA). While the development of AZT was groundbreaking, it needed to be taken at exact times around the clock, including in the middle of the night. This limited its effectiveness in countries where alarm clocks weren’t a daily part of life. AZT also cost about $9,000 a year—more than $21,000 when adjusted for inflation. But perhaps most important, AZT didn’t even guarantee survival—it could only delay the progression of AIDS.
Bill and Ernie Branson/National Institutes of Health via Flickr
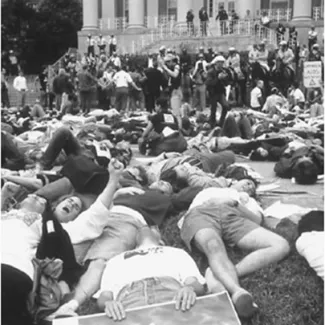
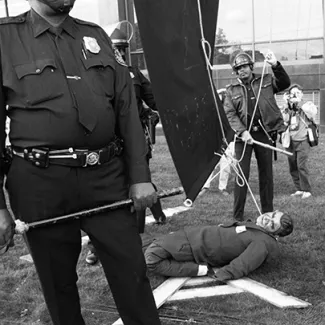
The AIDS advocacy group AIDS Coalition to Unleash Power (ACT UP) was formed; it would become one of the most prominent activist groups for people with AIDS (PWAs). ACT UP used drastic tactics to bring attention to the AIDS crisis. The organization notably shut down the Food and Drug Administration for an entire day in 1988. In 1990, 1,200 ACT UP protesters stood outside the National Institutes of Health to protest the use of placebos, the dearth of women and people of color in clinical trials, and other research practices they saw as unethical and against the interests of PWAs. Many of the PWA activists had become experts in the virus and shocked scientists with the extent of their medical knowledge.
Catherine McGann/Getty Images
President Reagan made his first public speech about AIDS and established the Presidential Commission on HIV. This commission was designed to investigate the AIDs epidemic and would later hear testimony from doctors, researchers, and activists. This was six years—and nearly twenty-five thousand deaths—after the start of the epidemic.
After over a decade of decentralized and sporadic reactions, public and media attention finally started shifting from stigma to outrage. Ryan White died in 1990 at the age of eighteen. His funeral was attended by well-known individuals including Elton John and then First Lady Barbara Bush. Public health funding began to shift to address the epidemic, as well. The Gates Foundation, created by Bill and Melinda Gates, became a pivotal donor. In 1998, the Gates family allocated $5,000 in grants toward AIDS research. Two years later, they were allocating nearly $78 million.
Wellcome Collection under CC BY-NC 4.0
Wellcome Collection under CC BY-NC 4.0

Jean-Marc Bouju/AP
Despite early progress with medications, the virus continued to spread. By 1994, AIDS was the leading cause of death for all Americans aged twenty-five to forty-four. By 1999, sub-Saharan Africa became the epicenter of the global epidemic: HIV patients occupied 50 to 80 percent of the hospital beds in the region. South Africa became the country with the highest absolute number of people living with HIV. While treatments continued to develop, their benefit was not shared equally across classes or continents.

Jeff Christensen/Reuters
After years of little to no international coordination, UNAIDS was launched to strengthen the United Nations’ response to the global AIDS epidemic. This program was a significant step at a time when there was little international coordination on the issue. Although the United Nations had been responding to AIDS already, UNAIDS was a consolidation of that response.
National Institute of Allergy and Infectious Diseases via Flickr under CC BY 2.0
This combination of three antiretroviral drugs not only stopped HIV from multiplying but also made it less likely to develop drug-resistant strains. However, the cost was still prohibitive for many patients. The annual cost for therapy could reach up to $31,000 ($53,000 in today’s dollars).

Mike Hutchings/Reuters
Meanwhile, in sub-Saharan Africa, antiretroviral drugs remained out of reach. Multinational pharmaceutical companies that held patents on the medicine refused to lower their prices in South Africa. As a result,the South African government passed a law allowing for the importation of the same drugs from countries where the price was lower. The same pharmaceutical companies—backed by the U.S. government—challenged the law in South African courts, which further delayed the process of getting the drugs to patients. The Treatment Action Committee, a group of South African activists inspired in part by the U.S.-based AIDS Coalition to Unleash Power (ACT UP), eventually succeeded in securing the availability of antiretroviral drugs in the public health-care system. This system provided healthcare to most of the South African Black community at the time. The ferocious battle over these drug patents caused a media firestorm, finally catching the attention of the public, the World Trade Organization, and most important, major donors.

Christine Wambaa/United Nations via Flickr under CC BY-NC-ND 2.0
The UN General Assembly passed the 2001 UN political declaration on HIV/AIDS. This declaration finally brought together countries to recognize the multifaceted AIDS crisis as “a paramount health, development, human rights, and social challenge.” It also called for the establishment of a better funding mechanism. Separately, the declaration paved the way for other international bodies such as the World Trade Organization to set international guidelines on issues such as drug distribution. But this was only the beginning. No global data was available on how many people had AIDS, especially outside the West. Meanwhile, the health-care gap between people with AIDS in countries such as the United States and South Africa only seemed to be widening.

Sebastian Derungs/Reuters
As governments around the world realized they needed to work together to effectively combat infectious diseases, the Global Fund to Fight AIDS, Tuberculosis, and Malaria was established in Switzerland. The organization was created to properly gather and channel the funding these diseases required. This coordinated effort represented one of the first steps in professionalizing the response to HIV/AIDS. UN Secretary-General Kofi Annan, who had called for such a fund, made the first donation. The Group of Eight (G8) countries soon followed suit, as did Bill Gates personally. The Global Fund would soon grow to become the lead funding mechanism for AIDS research.

Denis Farrell/AP
Twenty years after the virus first came into the public eye, President George W. Bush launched the President’s Emergency Plan for AIDS Relief (PEPFAR). This coordinated effort between the president’s office and eight U.S. federal agencies provided about $15 billion to prevent and treat HIV/AIDS to fifteen priority countries. These priority countries (twelve of which were in Africa) represented those hardest hit by HIV. Bush called it a demonstration of “compassionate conservatism.” For the first time, global programs such as PEPFAR and the Global Fund were working together to combat a single disease. Four years after PEPFAR was launched, global deaths from HIV/AIDS finally went down for the first time.

Mansi Thapliyal/Reuters
In the United States, the Food and Drug Administration approved Truvada for use as a pre-exposure prophylaxis (PrEP). It is not a vaccine but can be taken daily to lower the risk of infection. When PrEP was first developed and used as prescribed, it reduced the chance of HIV transmission from sex by 90 percent—more recent research puts the effectiveness at 99 percent. Some information also indicates that PrEP can reduce the risk of HIV from drugs by at least 74 percent. However, the average price of one PrEP treatment is nearly $2,000 for a thirty-day supply. The high price makes the treatment cost-prohibitive not only in the United States but also in developing countries where preventive care is most needed.

Denis Farrell/AP
In December 2020, the United Nations introduced their 95-95-95 plan. This plan aims for95 percent of people with HIV to know they are infected, access sustained antiretroviral care, and get viral suppression once on antiretroviral therapy by 2025. The plan was adopted by UN Members in June 2021. In the same year, approximately 85 percent of people knew they had the virus, 88 percent had treatment, and 92 percent were receiving viral suppression. Despite those successes, the world experienced the slowest decrease in infection rates since 2016 and an increase in thirty-eight countries.
Despite the progress made in reducing the spread of HIV, it should be remembered that the virus remains a present threat. In 2021, about 1.5 million people became infected with HIV worldwide. Experts believe nearly one in five people living with HIV don’t know that they’re HIV positive. Regions affected by HIV infection more recently haven’t seen the same reduction in transmission rates that the United States and sub-Saharan Africa have. In Central Asia and Eastern Europe, for example, the annual infection rate has risen by 48 percent between 2010 and 2021.
Citing general success, some policymakers have suggested cutting funding for AIDS programs such as the U.S. President's Emergency Plan for AIDS Relief (PEPFAR)—which celebrated twenty years in January 2023. PEPFAR is responsible for saving over twenty million lives since its inception. But donors such as Bill Gates, whose philanthropic organization has continued to contribute hundreds of millions of dollars to fighting HIV/AIDS, argue that complacency could lead to a mass resurgence of the virus. The story of AIDS has shown that each of those steps—from patient activism to medical research to unified international effort—is necessary to successfully combat the next infectious disease.

Vladimir Konstantinov/Reuters
Vladimir Konstantinov/Reuters








